What is Periodontal Disease?
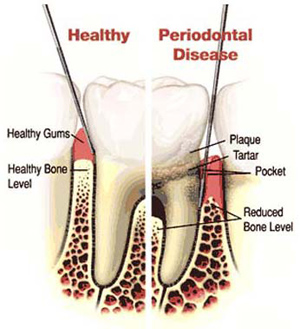
Periodontal disease, also known as periodontitis or gum disease is a bacterial gum infection that destroys the gums and the bone supporting your teeth. Research has shown that nearly one in three U.S. adults aged 30 to 54 has some form of periodontal disease. The main cause of periodontal disease is bacterial plaque, a sticky, colorless film that constantly forms on your teeth. If the plaque is not removed, it can turn into a hard substance called calculus or tartar in less than two days. Tartar can only be removed by a dentist or dental hygienist using special instruments. The bacteria found in plaque can infect the gums and release toxins that cause redness and inflammation in the gums. If they are not eliminated, the inflammation and the toxins can destroy the tissues that support the teeth, including the bone. When this happens, the gums separate from the teeth, forming pockets that fill with even more plaque; causing more infection.
What causes periodontal disease? Periodontal disease is usually caused by a number of factors. The most common causes of periodontal disease include:
- Smoking can significantly increase the risk of developing periodontal disease and can negatively affect treatment outcomes.
- Hormonal changes during pregnancy, puberty and menopause can cause the gums to become red, swollen and bleed easily.
- Genetics and a family history of periodontal disease indicate a greater likelihood of developing this disease.
- Stress can make it more difficult for the body to fight off infection, including periodontal disease.
- Medications such as oral contraceptives, antidepressants and certain heart medicine, can affect oral health.
- Destructive habits such as improper oral home care, oral piercing, drug or alcohol abuse can affect periodontal health.
- Poor nutrition can make it harder for the body to fight off infections.
What are the signs and symptoms of periodontal disease? Periodontal disease is often silent, meaning that symptoms may not materialize until significant bone loss has already occurred. Some people may have periodontal disease and not experience any symptoms and be unaware that they have disease. Common symptoms and signs of periodontal disease include:
- Red, swollen or tender gums
- Bleeding while brushing or flossing
- Gums receding or pulling away from the teeth making the teeth appear longer
- Loose or separating teeth
- Pus between the gum and tooth
- Persistent bad breath
- A change in the way your teeth fit together when you bite
- A change in the fit of partial dentures
During your periodontal examination, we will gently place a small measuring instrument called a periodontal probe in the pocket between the teeth and gums to measure pocket depths. Probing depths measuring 1-3 mm without bleeding or gum recession are typically considered healthy. Four mm pockets with bleeding may indicate gingivitis or possibly even early periodontal disease. Five mm+ pockets with multiple bleeding sites strongly indicate the presence of bacterial infection or moderate to severe periodontal disease.
How is periodontal disease diagnosed and treated? Measuring the pockets surrounding your teeth, evaluating the health of your gums, and reviewing your X-rays is the most reliable way to determine your periodontal health. Once your periodontal health has been evaluated, your treatment can vary depending on how far the disease has progressed. If diagnosed and treated in the early stages, simple non-surgical periodontal therapy, such as scaling and root planing, may be sufficient. If periodontal disease has advanced to the point where the periodontal pockets are deep and significant amounts of bone are lost, surgical therapy may be necessary.
Once periodontal disease has been controlled, patients will require ongoing periodontal maintenance to sustain health. This ongoing phase of treatment will allow us to assess your periodontal health and make sure that your infection stays under control or remains eliminated. During these re-evaluation appointments, your mouth will be examined, infected areas that are not accessible by brushing and flossing will be thoroughly cleaned with special instruments and, if necessary, your teeth will be polished and your bite checked. The infection must be removed every 90-120 days to prevent further irritation to your gums and to prevent further destruction of bone. Just like diabetes, periodontal disease is a chronic disease. Without careful, ongoing treatment, periodontal disease can and often does recur.
What is scaling and root planing (SRP)? Scaling and root planing (SRP) is a thorough cleaning of the root surfaces below the gum line to remove plaque, toxins and tartar from the root surfaces of the teeth. This procedure is more intensive than a routine dental prophylaxis, or cleaning, which traditionally occurs every six months.
For your comfort, we may numb the area prior to treatment. Research has consistently shown that SRP reduces gingival inflammation and pocket depths, and shifts the types of bacteria living in these pockets from one that is associated with disease toward one associated with health. That is why SRP is usually the first treatment recommended for most periodontal patients.
In some cases, systemic antibiotics (usually antibiotic pills taken orally) or locally-administered antibiotics (antibiotics placed directly into periodontal pockets to suppress or eradicate periodontal bacteria) may be prescribed at the time of the SRP procedures.
My insurance only covers two cleanings a year. How does my insurance work if I need to come back in three to four months for a periodontal re-evaluation? It is true that most dental plans allow two cleanings a year for healthy patients. For patients with periodontal disease, however, you have separate benefits aimed at arresting bacterial infection and preventing further bone loss. Depending on the premiums paid by you and/or your employer, periodontal benefits usually range from 30-80 percent. A deductible may also apply.
Once you have been diagnosed with periodontal disease, we are obligated to provide your dental plan with the appropriate billing codes, a copy of your periodontal measurements, and some X-rays. Legally and ethically, as your dental providers, we cannot ignore the bacterial infection in your mouth simply because of insurance limitations that may exist. With periodontal disease the risk is too great. Whatever dental insurance you have, you can rest assured that we will do our best to see that you receive the dental benefits provided to you.
How can periodontal disease be prevented? Good oral hygiene and professional care are the keys to keeping your teeth for a lifetime. The best way to prevent periodontal disease and tooth decay is to remove the bacterial plaque by thorough brushing and flossing every day. Good oral home care habits will help keep the formation of dental tartar to a minimum. Regular dental checkups that include a periodontal examination are also important to detect any changes in periodontal health and, if necessary, to remove hardened tartar in places that your toothbrush and floss may have missed. A professional cleaning at least twice a year is recommended for patients with good periodontal health. If you have had any form of periodontal disease, you may need professional maintenance more frequently.
Is there a link between diabetes and periodontal disease? Yes. Diabetic patients are three-to-four times more likely to develop chronic periodontal disease.
Like any other infection in the body, periodontal infections can interfere with the body's ability to process and/or utilize insulin which can make diabetes more difficult to control. In addition, a periodontal infection may be more severe in a diabetic patient than in someone without diabetes. That is why it is important for diabetic patients to have their periodontal disease treated to control or eliminate the infection as one more way to achieve optimal control of their blood sugar levels.
Is there a link between heart disease and periodontal disease? Recent studies suggest that people with periodontal disease may have nearly twice the risk of having a fatal heart attack as those without periodontal disease.
There are several reasons why periodontal bacteria may affect your heart. In the presence of gum disease, normal tasks such as chewing or brushing your teeth may allow bacterial toxins to enter the bloodstream and irritate the blood vessel lining and/or increase the chances that small blood clots will form and clog your arteries.
Another possibility is that the inflammation caused by periodontal disease may release chemicals into your blood that contribute to the buildup of fatty deposits inside your heart arteries.
Like high cholesterol, an elevated level of C-reactive protein (CRP) could be another reason as to why periodontal disease could be a risk factor for heart disease. Periodontal disease appears to trigger the liver to make proteins such as CRP that inflame arteries and cause blood clots that can lead to heart attacks.
Can periodontal disease contribute to pregnancy complications? During pregnancy, your body experiences hormonal changes. These changes can affect many of the tissues in your body, including your gums. Your gums may become sensitive, and at times may react strongly to the hormonal fluctations. Without proper care and treatment, relatively mild gum problems may turn into a more advanced form of periodontal disease.
In recent years, studies have indicated that women who experience periodontal disease progression during their pregnancies may be twice as likely to develop preeclampsia (high blood pressure and the presence of protein in the urine) as a complication of pregnancy. Preeclampsia can put you and your baby at risk for severe complications. In addition to preeclampsia, periodontal disease can trigger increased levels of biological fluids which can induce preterm labor.
Studies have also suggested that women whose periodontal conditions worsen during pregnancy are at a significant risk of having a premature or low birth weight baby. In fact, pregnant women who have periodontal disease may be up to seven times more likely to have a baby who is born too early and too small.
The good news is that several studies have found that treating periodontal disease during pregnancy may significantly reduce the risks of a preterm birth. Preventing gum problems from developing during the stresses of pregnancy also appears to be important in improving the health of the mother and baby.
Is there a link between respiratory diseases and periodontal disease? Bacterial respiratory infections can be acquired by the inhalation of tiny bacteria-filled droplets from the mouth and throat and into the lungs. Periodontal disease, which is a bacterial infection, may be a major factor in the development of bacteria that are found in fluid droplets in the lungs. Once the bacteria are in the lower respiratory tract, they multiply causing infections or worsening of existing lung conditions. An individual with periodontal disease may be more likely to develop respiratory diseases like Chronic Obstructive Pulmonary Disease (COPD) which can decrease lung function.
175 N. Milwaukee Avenue, Suite 200
Vernon Hills, IL 60061
(847) 955-9500
Email Us
Copyright ©2025 Arbor Hills Dental Care, P.C. All Rights Reserved.
